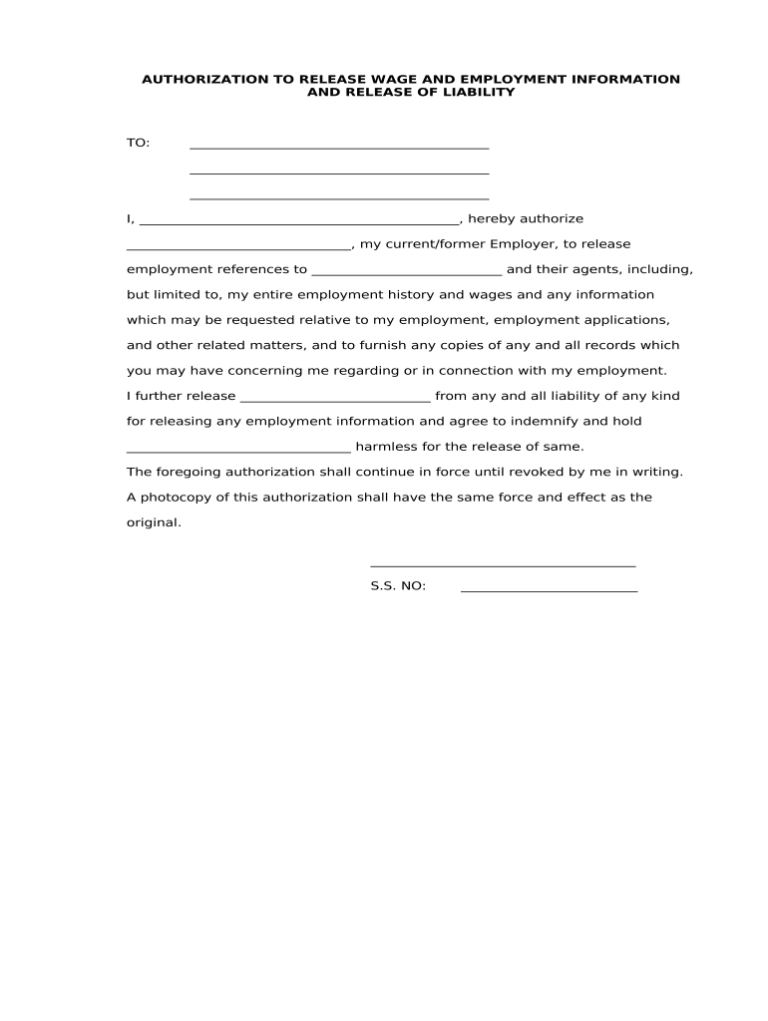
There are several benefits to using an authorization for prior employer to release information template. First, it can save you time and effort. By providing your potential employer with a signed authorization, you can avoid having to contact your previous employer yourself and request that they release your information. Second, it can help you to ensure that your potential employer receives accurate and complete information about your work history. By signing an authorization, you are giving your previous employer permission to release all relevant information, even if it is negative. This can help to ensure that your potential employer has a clear understanding of your strengths and weaknesses.
prior
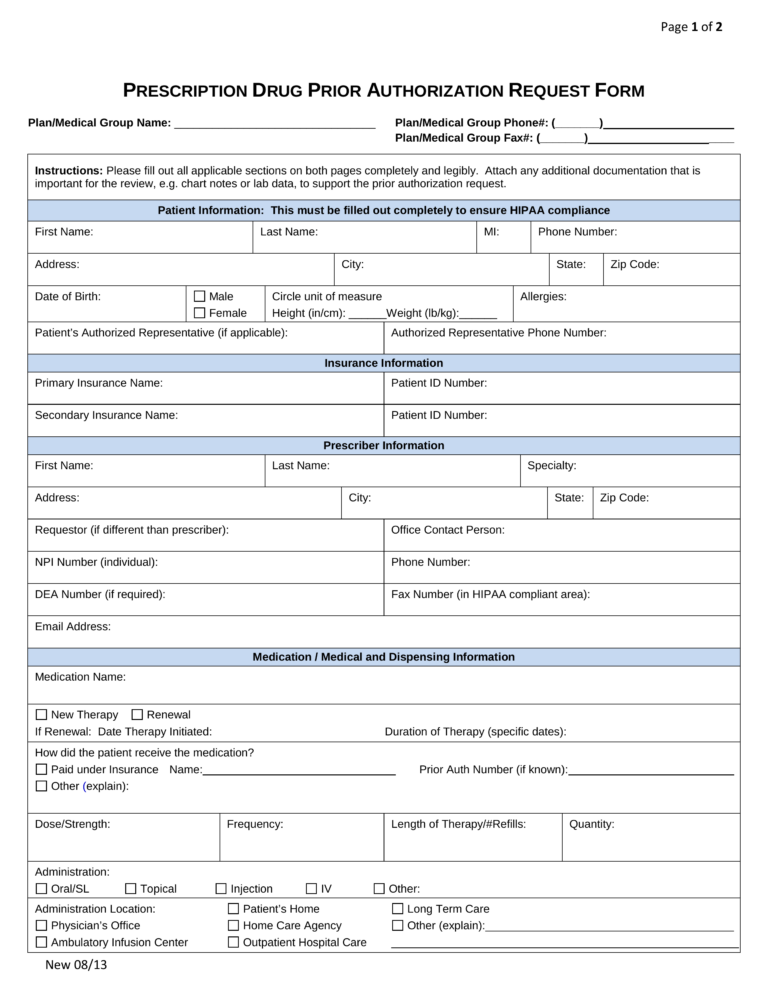
Prior Authorization Cheat Sheet Template
- The patient’s name and insurance information
- The medication or treatment being requested
- The diagnosis or condition being treated
- The reason for the request
- The supporting documentation that is required
Using a prior authorization cheat sheet template can save providers time and hassle. It can also help to ensure that all of the necessary information is included in the request, which can increase the likelihood of approval.
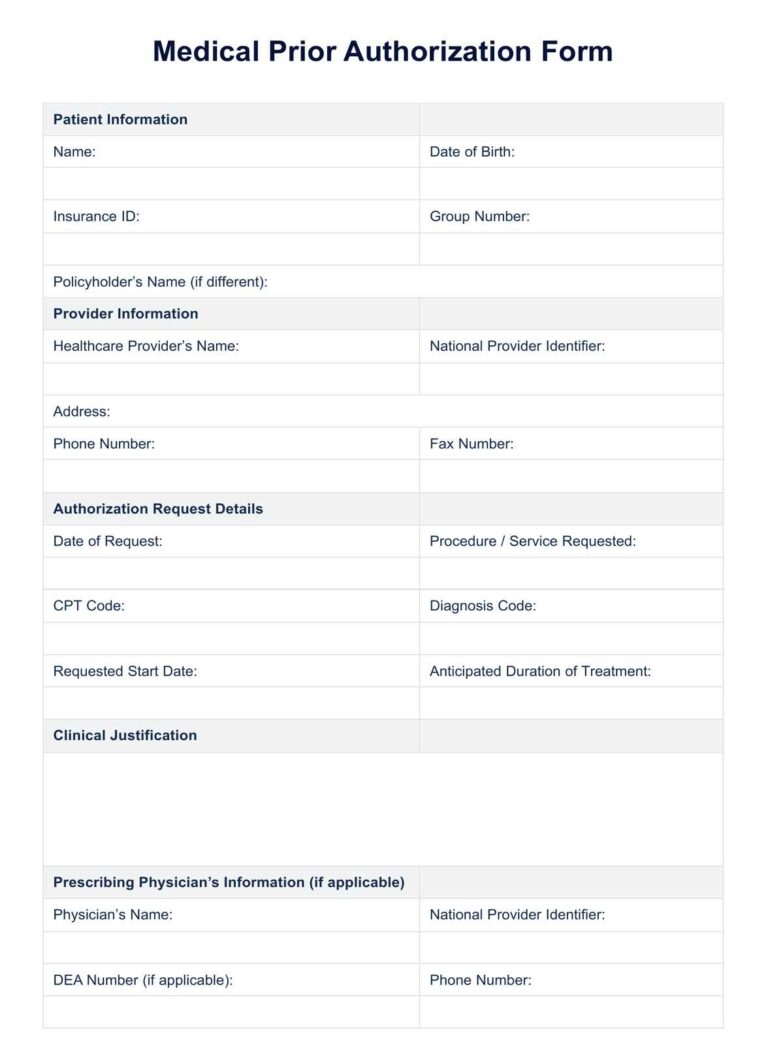
Medical Prior Authorization Form Template
There are many benefits to using a medical prior authorization form template. These benefits include:
Insurance Prior Authorization Form Template
There are several benefits to using an insurance prior authorization form template. First, it can help to ensure that the patient receives the necessary care in a timely manner. Second, it can help to reduce the cost of the patient’s care by ensuring that the insurance company approves the most cost-effective treatment plan. Third, it can help to protect the healthcare provider from being held liable for providing unauthorized services.
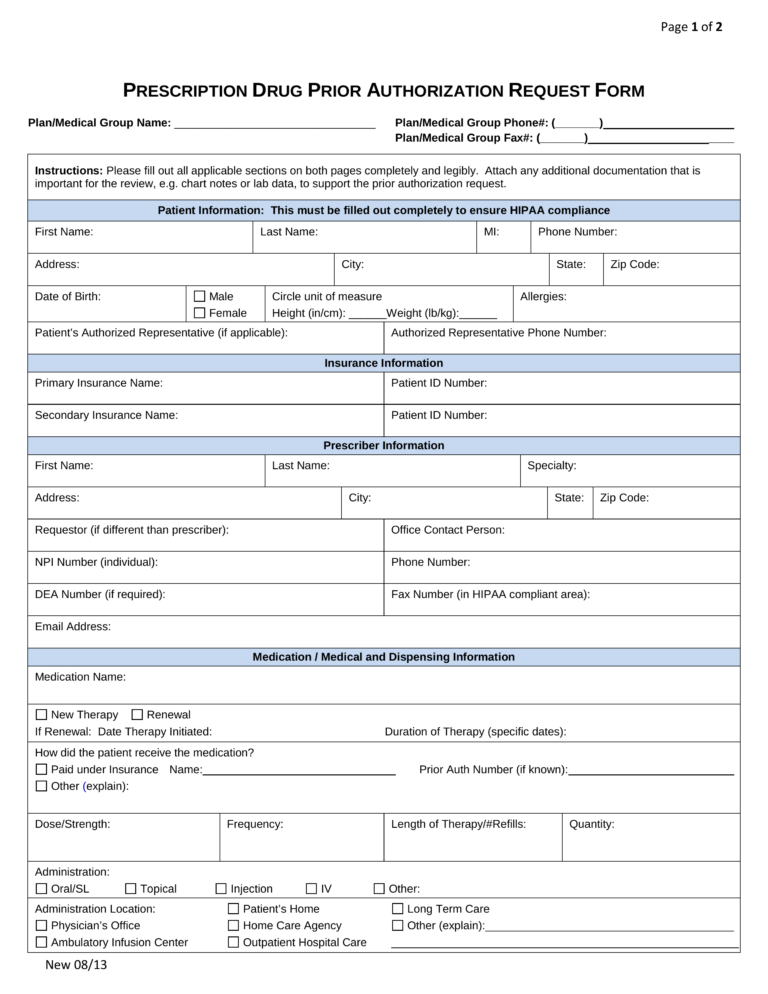
Generic Prior Authorization Form Template
There are many benefits to using a generic prior authorization form template. First, it can help to streamline the prior authorization process by ensuring that all of the required information is submitted to the insurance company in a standardized format. This can help to reduce the amount of time that it takes to get approval for treatment, which can be crucial for patients who need urgent care. Second, using a generic template can help to improve the accuracy of prior authorization requests. By providing a clear and concise format, healthcare providers can reduce the likelihood of errors that could delay or even deny approval for treatment.
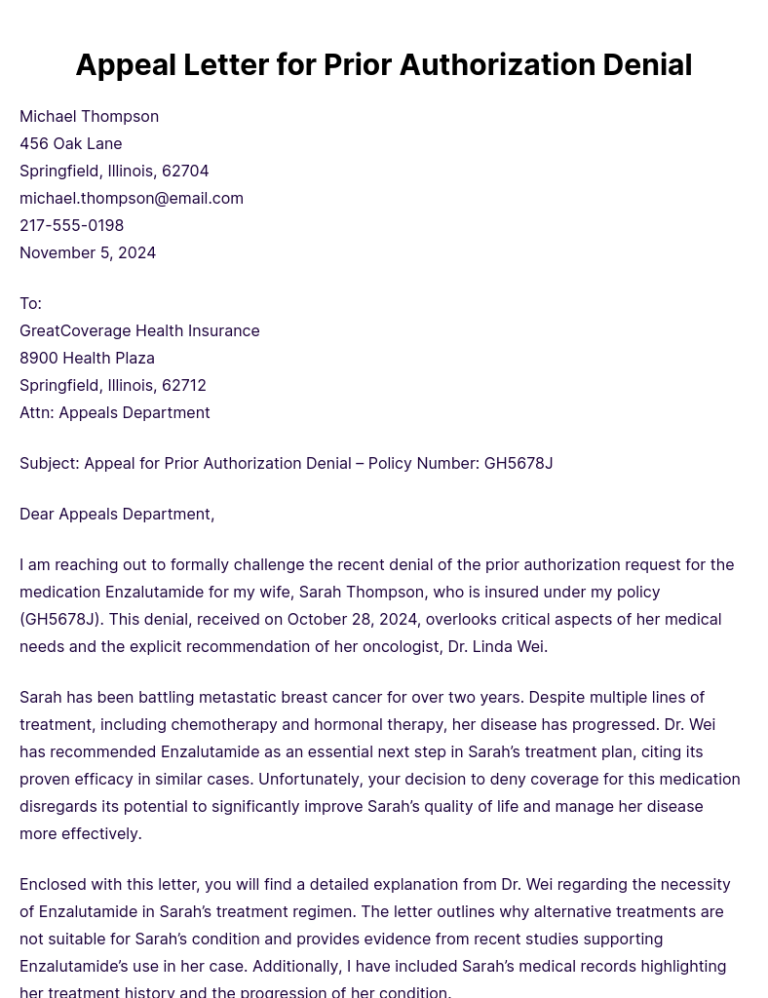
Prior Authorization Appeal Letter Template
There are many benefits to using a prior authorization appeal letter template. First, it can help to ensure that the letter is complete and includes all of the necessary information. Second, it can help to organize the letter in a logical way, making it easier for the insurance company to review. Third, it can help to save time, as the letter can be easily customized to fit the specific needs of the individual.
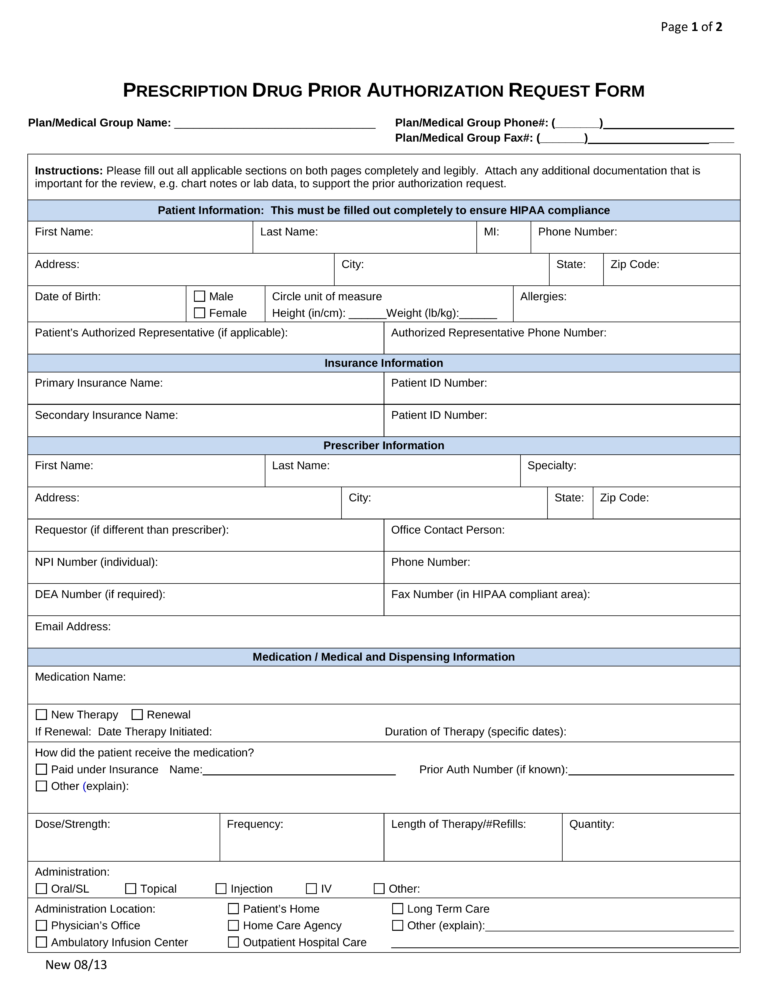
Printable Medical Prior Authorization Form Template
Benefits of Using a Printable Medical Prior Authorization Form Template
Using a printable medical prior authorization form template offers several benefits for healthcare providers and patients: